
Measles in the city. Main regularities of the epidemic process in different strategies for prevention and control of the situation in modern conditions
Alla Golubkova1,3, Tatiana Platonova, Olga Olshvang, Svetlana Smirnova1,3, Svetlana Kovyazina5, Angela Paraschiv6
1Department of epidemiology, Ural State Medical University, Yekaterinburg, Russian Federation;
2Department of foreign languages, Ural State Medical University, Yekaterinburg, Russian Federation;
3Ural and Siberian scientific methodological center for HAI prevention, Yekaterinburg Research Institute of Viral Infections of Rospotrebnadzor, Yekaterinburg, Russian Federation;
4UMMC-Health LTD, Yekaterinburg, Russian Federation;
5Department of epidemiological surveillance, Directorate of Rospotrebnadzor in the Sverdlovsk region, Yekaterinburg, Russian Federation;
6Chair of epidemiology, Nicolae Testemitanu State University of Medicine and Pharmacy, Chisinau, Republic of Moldova.
Autor corespondent:
Alla Golubkova, PhD
Department of epidemiology
Ural State Medical University
3, Ilya Repin str., Yekaterinburg, Russian Federation
e-mail: allagolubkova@yandex.ru
Short title of the article: The epidemic process of measles in the city
What is not known yet, about the topic?
To date, no comprehensive detailed study of the epidemic process of measles was conducted from the period before vaccination to the elimination of the infection in the city, and the features of the formation of the outbreaks were not assessed at the stage of elimination of the infection.
Research hypothesis
The study of the determinants of the epidemic process of measles in the large city in the historical context allows developing measures to control the situation in modern conditions.
Article`s added novelty on this scientific topic
In the process of the study the incidence of measles was retrospectively analyzed in a large industrial city for 67 years and the interventions to control the epidemic process at the present stage were suggested.
ABSTRACT
Introduction. Measles infection is still relevant in connection with the registration of the outbreaks of this disease in different territories. The purpose of the research was to characterize the epidemic process of measles in a large industrial city in terms of different strategies for its vaccination, in order to adopt new administrative decisions on infection control at the stage of its elimination.
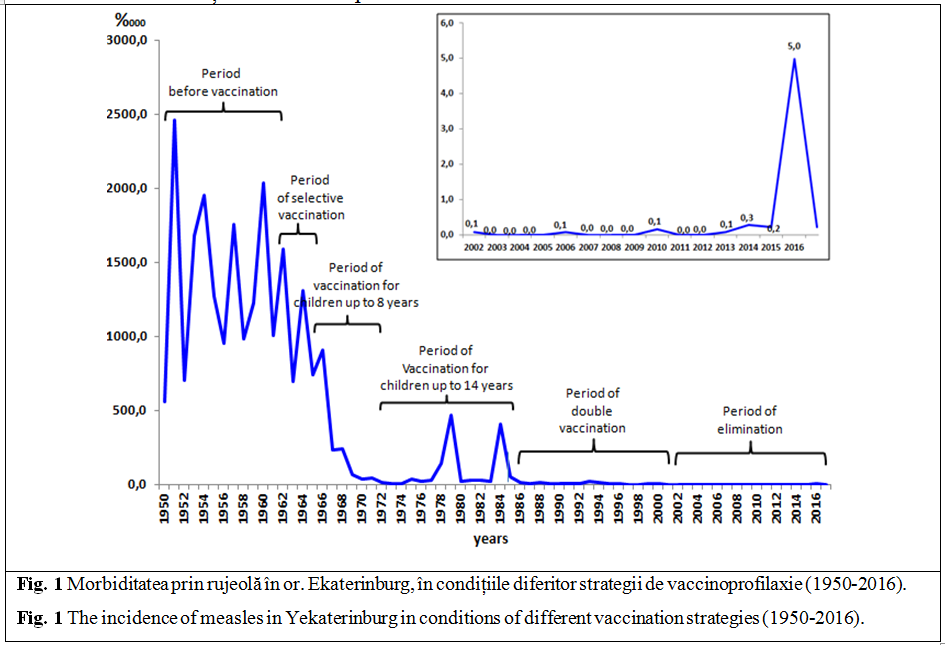
Material and methods. The research is based on data of statistical reports on the incidence of measles in Yekaterinburg from 1950 to 2016. The manifestations of the epidemic process were analyzed for six periods: the period before vaccination (1950-1961), the period of selective immunization (1962-1965), routine vaccination of children up to 8 years (1966-1972), routine vaccination of children up to 14 years (1973-1986), the introduction of mass revaccination of children (1987-2001) and the period of the generalized vaccination at the stage of elimination of the infection (2002-2016).
Results. In the period before vaccination, the mean annual incidence was 1381.7±162.90/0000, the seasonal rise of incidence was in December-May, children prevailed in the structure of the age groups. In the period of selective immunization, there was a slight decline in the incidence to 1082.8±189.10/0000, the dynamics within the year and the age distribution of cases were similar to the period before vaccination. During vaccination of children up to 8 years, there was a significant decrease in morbidity to the level of 219.8±110.80/0000, which was observed in almost all age groups except for children aged 10-14 years and adults. Seasonal manifestations of the epidemic process were similar to the previous periods. During vaccination of children up to 14 years, there was a further decrease in the incidence of 89.9±39.10/0000, but in some years, the outbreaks of the infection were reported. The introduction of the second vaccination to children aged 6 years before school allowed us to achieve the sporadic incidence and to change the basic parameters describing the epidemic process in all previous periods. However, against this background, a measles outbreak was reported in 2016 when 72 people were affected. The outbreak was caused by the introduction and spread of measles virus of genotype D8 mainly in the medical settings among unvaccinated children and adults.
Conclusion. At the present stage, in order to control the epidemic process of measles, it is necessary to redefine the criteria for the evaluation of epidemiological safety of the territory in terms of expansion of indications for screening for antibodies to measles among patients with exanthema, strict control of timeliness of immunization of the decreed population (children aged 1 year and 6 years) and the introduction of routine revaccination of persons under the age of 50 years every 10 years.
Keywords: measles, epidemic process, the strategy of vaccination.
INTRODUCTION
Until the mid-20th-century measles was the most common pediatric infection, the incidence of which was identical to the birth rate. In 1967 the introduction of vaccination against measles in the healthcare practice significantly changed the situation: the incidence, lethality and mortality from this infection decreased, there were changes in the age distribution of cases and focality [1-5].
Due to the constant increase in vaccination coverage of the population, in the late 20th – the early 21st century there was a steady downward trend in the incidence in most countries of the world and even the cessation of virus circulation in particular periods of time [1-5].
However, since 2013, some countries have reported an increase in the incidence of measles with active involvement of adolescents and adults in the epidemic process, with outbreaks of measles in groups and focality. In some administrative territories of the Russian Federation, the cases of measles introduction were also recorded with the spread and the formation of the epidemic foci with multiple illnesses in the families, medical settings and educational institutions [6-11].
The situation for measles requires further study of the manifestations of the epidemic process in the historical perspective, identifying its main patterns and determinants, in order to improve the system of epidemiological surveillance and infection control at the stage of its elimination. The purpose of the research was to characterize the epidemic process of measles in a large industrial city in terms of different strategies for its vaccination, in order to adopt new administrative decisions on infection control at the stage of its elimination.
MATERIAL ȘI METHODS
The research was performed in 2017-2018 at the Department of epidemiology of the Ural State Medical University.
In the research, the data of statistical reports on the incidence of measles in Yekaterinburg from 1950 to 2016 were analyzed. The explanatory note to the annual reports of the sanitary and epidemiological stations "On the movement of infectious diseases", f. 85 (39), forms of Federal state statistical observation no. 1, 2 "Information about infectious and parasitic diseases" (60), as well as emergency notices, f. 058/y (1221).
A study of the annual dynamics of the incidence and morbidity of certain age groups within a year was carried out for six periods: the period before vaccination (1950-1961), the period of selective immunization (1962-1965), routine vaccination of children up to 8 years (1966-1972), vaccination of children up to 14 years (1973-1986), the introduction of mass revaccination of children (1987-2001) and the period of the generalized vaccination of children and adults at the stage of elimination of the infection (2002-2016).
The mean annual incidence, the average annual rate of growth/reduction of morbidity were calculated to characterize the epidemic process. The index of the standardized range (estimated Hurst exponent) was used to assess the degree of stochasticity of the time series of incidence. The number was considered to be anti-persistent, if H<0.5 (the rise was followed by the decline, the decline was followed by the rise); with a stable trend if 0.5<H≤1.0 (the rise was followed by the rise, the decline was followed by the decline). When N=0.5, the trend of the dynamics of the process was considered to be uncertain or random.
The study used epidemiological and statistical research methods. The research was retrospective. The conventional statistical techniques were used for the evaluation of the results. The calculations were carried out using the software package Microsoft Office 2007. The significance of differences was assessed by the student's test. The differences were considered to be significant at p<0.05.
RESULTS
The periodicity in the incidence of measles (Figure 1) was observed in the period before vaccination on the territory of the city. The years of the rise were followed by the years of decline, the interval between the periods of rise in incidence was 1-2 years. In 1950-1961 the mean annual incidence was 1381.7±162.9 per 100 thousand people and was equal to the birth rate.
The trend curve of incidence over the studied period suggested the presence of a stabilizing trend in the alternation of epidemic waves (T= +0.1%). The estimated Hurst exponent was 0.472, which allowed characterizing the dynamics of infection as anti-persistent.
The incidence began to increase in September, reaching a maximum level in February, then there was a gradual decrease until August. When analyzing the age structure of cases, it was established that measles were reported in all age groups of children and adults up to 30 years in the period before vaccination. Among the cases, the vast majority was children (99.7±0.05%); adults had only isolated cases of measles (0.3±0.01%).
In 1962, live measles vaccine started to be used for immunization of limited groups of children, in terms of epidemiological experience in the city. There was a slight decrease in the incidence under the influence of vaccination in this period (Figure 1). The average annual incidence was 1082.8±189.10/0000. For the first time in this period, it tended to decline, with an average annual rate of decline -17.9%, which is confirmed by the quantitative evaluation of the index of standardized range (0.644). The frequency, seasonality and age distribution of cases corresponded to the period before vaccination.
Since 1966, the city began planning the vaccination of children up to 8 years of age. An evident trend towards a reduction in morbidity was observed in the period of routine vaccination (Figure 1). The average annual rate of reduction was -53.0%. The estimated Hurst exponent equal to 0.529 allowed to characterize long-term dynamics of morbidity as a stable trend within these years. The mean annual incidence rate was 219.8±110.80/0000, which is 6.3 times lower compared to the period before vaccination (t=5.9, p<0.05). The decline in incidence rates was reported in almost all age groups, except groups of children aged 10-14 years and adults, among which there was even some increase in morbidity (4.9±0.2 vs. 1.9±0.09 per 1,000 children aged 10-14 years and 0.5±0.02 vs. 0.3±0.01 per 1,000 adults). Compared to previous periods the dynamics of morbidity within a year remained unchanged.
In 1973, a decision was made on the prolongation of the age for vaccination to 14 years as a remedial action. The incidence dropped to 89.9±39.10/0000 as a result of immunization coverage of children in older age groups. However, its significant rises were reported in some years of this period (1979 and 1984), with the active involvement of persons over the age of 7 years in the epidemic process, the outbreaks in schools and other educational institutions. In this period the incidence of measles became anti-persistent again (H=0.381).
The distribution of measles cases within a year differed from that in previous years. April was the month with the highest average daily number of cases, and September was the month with the lowest number of cases. The seasonal rise had two waves: the first wave was in January-February, the second one was in March-April. In the analysis of the age-specific distribution of cases, a further decrease in the incidence of measles was established in age groups of up to 10 years. There was a tendency to incidence rise among children aged 10-14 years and adults.
In 1987, the introduction of revaccination against measles aimed to correct defects of primary vaccination resulted in a significant reduction in the intensity of the epidemic process (Figure 1). The mean annual incidence decreased to 5.7±1.60/0000, which was significantly lower than in all previous periods (t>2, p<0.05). However, in some years there was still an increase in incidence, although it was small (in 1988, 1991, 1993, and 2000). The frequency of incidence ranged from one year up to 4 years.
The estimated Hurst exponent was 0.381 which confirmed anti-persistent morbidity, the alternation of rising and decline. Overall in this period, there was a downward trend in incidence with an average annual rate of decline -6.1%. In the dynamics, within a year there was a shift in the seasonal rises of morbidity to February-June, and adults began to prevail in the age structure.
In the period of elimination of the infection (2001-2015), the incidence corresponded to a sporadic level (0.06±0.020/0000); there was an isolated introduction of measles from other regions but without infection spread. The infection was introduced from other territories of the Russian Federation (Moscow, Sankt Peterburg, Kemerovo region) as well as from other countries (Ukraine, Kyrgyzstan, Uzbekistan, Croatia, Sri Lanka). For 15 years there were only 12 clinically and laboratory-confirmed cases of measles.
However, after many years of absence of indigenous measles in 2016 in Yekaterinburg, there was an outbreak of infection with 72 cases (5.0±0.60/0000). In the age structure of cases there have been children and adolescents up to 18 years (68.1%), the adults accounted for 31.9%. The average age of affected children was 3.8 years; the average age of affected adults was 33.2 years. No differences were found in the gender profile of cases of measles.
As for the vaccination history, 68.1% of patients were not previously vaccinated against measles, including by reason of refusal of vaccination (38.8%), medical contraindication (34.7%), and age (16.3%). In 10.2% of cases, the vaccination history was not known. Among the cases of measles in previously vaccinated people, 30.4% were vaccinated once, 47.9% were vaccinated twice and 21.7% were vaccinated three times.
Laboratory tests using ELISA in all patients revealed class M specific antibodies. When examined using the PCR method, the antigen of measles virus of genotype D8 was isolated, which had been circulating in South-East Asia in previous seasons, and it was in Europe and Russia in season 2015.
During the outbreak, 59 local foci emerged with different numbers of affected persons, including 36 family housing, 14 persons in the organized groups and 9 cases in medical settings. The most active spread of the infection took place in medical settings, where the focality index was 7.1, the focality rate was 55.6%, and the reproduction rate of the infection reached 10.2. The spread of the infection in medical settings was linked to the presence of children and adults who had not been previously vaccinated against measles, late diagnosis of measles in the first and subsequent cases and violations of anti-epidemic measures in the institution.
CONCLUSION
Under the influence of vaccination, the epidemic process of measles has undergone significant changes: the incidence has decreased; the frequency, the seasonality of infection and the age structure of cases have changed. However, in the context of long-term routine vaccination, the possibility of outbreaks of measles among unvaccinated children and adults remains which requires rethinking the criteria for the evaluation of epidemiological safety of the territory in terms of expansion of indications for screening for antibodies to measles among patients with exanthema, strict control of timeliness of immunization of the decreed population (children aged 1 year and 6 years) and the introduction of routine revaccination of persons under the age of 50 years every 10 years. The issue of inconsistency of genotype of "wild" measles virus which caused outbreaks of measles in recent years and vaccine measles virus shall be studied.
Declaration of conflicting interests
The authors declare no potential conflict of interest that may have a direct or indirect impact on the process of preparation or publication of the article.
Authors’ contribution
All authors had equal contributions to the research and writing of the manuscript.
Acknowledgment
The authors acknowledge the assistance of staff of the Central Yekaterinburg Department of Rospotrebnadzor in the Sverdlovsk region (Losevskaya O., Nesgovorova G.) and the Central Yekaterinburg branch of Center of hygiene and epidemiology in the Sverdlovsk region (Karimova N.) in gathering material for the research.
REFERENCES
- Tsvirkun O. The epidemic process of measles in different periods of vaccination: Abstract of Doctor of Medical Sciences thesis. Moscow; 2014. http://www.crie.ru/pdf/avtoref1(tsvirkun).pdf.
- Tsvirkun O., Tikhonova N., Yushchenko G., Gerasimova A. The epidemic process of measles in different periods of vaccination. Epidemiology and Vaccine Prevention, 2015; 2 (81): 80-87. https://www.epidemvac.ru/jour/article/view/43.
- Tsvirkun O., Gerasimova A., Tikhonova N., Turaeva N., Pimenova A. The structure of cases of measles in the period of elimination. Epidemiology and vaccine prevention, 2012; 2: 21-25. https://www.epidemvac.ru/jour/article/view/342.
- National action plan for the implementation of the program "Elimination of measles and rubella in the Russian Federation" (2016-2020). http://rospotrebnadzor.ru/deyatelnost/epidemiological-surveillance/?ELEMENT_ID=5968.
- The program "Elimination of measles and rubella in the Russian Federation" (2016-2020). http://rospotrebnadzor.ru/deyatelnost/epidemiological-surveillance/?ELEMENT_ID=5968.
- Golubkova A., Platonova T., Kharitonov A., Rybinskova E., Lelenkova E., Yuzhanina T. Measles. Characteristic of epidemic process and its determinants in real time (the case of measles outbreak in Yekaterinburg in 2016). Epidemiology and Vaccine Prevention, 2017; 6 (97): 54-58. https://www.epidemvac.ru/jour/article/view/342.
- Golubkova A., Platonova T., Kharitonov A., Sergeev A., Lelenkova E., Yuzhanina T. The epidemic process of measles in the period of its elimination and strategic direction for monitoring in real-time. Perm Medical Journal, 2017; 4: 67-73. https://journals.eco-vector.com/PMJ/article/view/6977.
- Scriabina S., Kovyazin S., Kuzmin S., Yurovskikh, A., Tsvirkun O., Gerasimova A. et al. The measles outbreak in the Sverdlovsk region. Epidemiology and Vaccine Prevention, 2017; 2 (99): 50-56. https://www.epidemvac.ru/jour/article/view/430.
- Werber D., Hoffmann A., Santibanez S., Mankertz A., Sagebiel D. Large measles outbreak introduced by asylum seekers and spread among the insufficiently vaccinated resident population, Berlin, October 2014 to August 2015. Eurosurveillance, 2017; 22 (34): 1-8. https://www.ncbi.nlm.nih.gov/pubmed/28857043.
- Magurano F., Baggieri M., Filia A., Manso M., Lazzarotto T., Amendola, A. et al. Towards measles elimination in Italy: Virological surveillance and genotypes trend (2013-2015). Virus Research, 2017; 236: 24-29. https://moh-it.pure.elsevier.com/en/publications/towards-measles-elimination-in-italy-virological-surveillance.
- Gibney K., Brahmi A., O’Hara M., Morey R., Franklin L. Challenges in managing a school-based measles outbreak in Melbourne, Australia, 2014. Australian and New Zealand Journal of Public Health, 2017; 41: 80-84. https://www.ncbi.nlm.nih.gov/pubmed/27960246.
